Certain medications have the potential to affect a person’s sleep. Some drugs help people sleep better. However, many medications, from cold and flu remedies to cancer treatments, can cause insomnia, making it hard to fall or stay asleep.
Some people develop insomnia after they start a medication or during the withdrawal period after they stop taking a drug. In 2016, over 17% of American adults reported taking at least one drug that listed sleep disturbances as a side effect.
In addition to causing insomnia, some medications affect sleep architecture, or how the sleep cycle is structured. During healthy sleep, people cycle through three stages of non-rapid eye movement sleep and one stage of rapid eye movement (REM) sleep multiple times each night. Disrupted sleep architecture is often associated with sleep disorders and health problems.
We describe common medications that may cause insomnia or disrupt sleep architecture. These medications include over-the-counter products, prescription drugs, and dietary supplements. If you are currently taking any medications that affect your sleep, it is important to address your concerns directly with your doctor prior to making any changes.
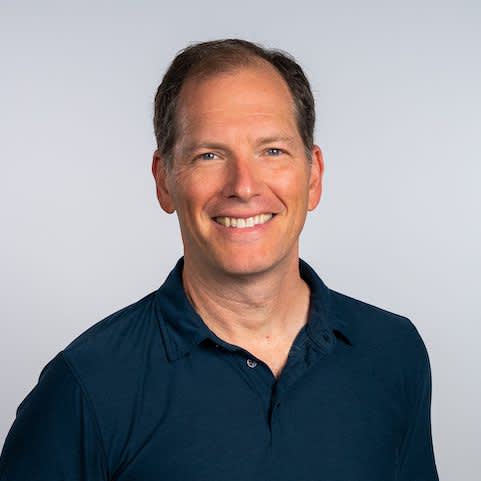
Get Personalized Advice from a Certified Sleep Coach

Sleep Doctor Adult Sleep Coaching
Sleep Doctor Adult Sleep Coaching pairs each client with a certified sleep coach. During your four to six one-on-one sessions, you’ll receive personalized tips and guidance based on your specific sleep needs.
Cold and Allergy Medications
Over-the-counter cold medications often contain a decongestant drug called pseudoephedrine, which can reduce nasal congestion. Pseudoephedrine is known to cause insomnia, even when it is used in the form of a nasal spray.
Some allergy medications called antihistamines promote sleep, so pseudoephedrine may be added to them to prevent drowsiness. As a result, antihistamines that are marketed as “non-drowsy” or containing a decongestant may interfere with sleep.
Sometimes, doctors prescribe steroid medications called corticosteroids to individuals with severe allergies. Corticosteroid inhalers and nasal sprays are unlikely to affect sleep in most people, but many oral steroid drugs are known to keep those who take them awake at night.
Although insomnia is not a listed side effect of the cough suppressant dextromethorphan, this drug can trigger restlessness and agitation. Some people may experience trouble sleeping as a result.
SSRI Medications (Antidepressants)
Whether they cause drowsiness or insomnia, most antidepressants affect sleep. Doctors may prescribe a type of antidepressant, called a selective serotonin reuptake inhibitor (SSRI), for insomnia. However, it is not clear how effective these medications are at helping people sleep.
Like other types of antidepressants, SSRIs lengthen stage 1 sleep and reduce REM sleep. Stage 1 is the lightest phase of the sleep cycle, when the sleeper is easiest to wake. This may be why SSRIs cause some people to wake up frequently in the night and sleep for fewer hours in total.
While a few studies suggest that SSRIs might help some people sleep better, reactions appear to be mixed and depend on which drug the individual is taking. Certain SSRIs seem more likely to cause insomnia than others. People may also experience sleep issues if they abruptly stop taking an SSRI without tapering off their dosage.
Beta Blockers (Blood Pressure Medications)
Beta blockers treat high blood pressure by slowing the heart rate. Some beta blockers are fat soluble, which means that they are stored in the body’s fats and tissues. Others are water soluble and stay within the blood and surrounding fluids. Water-soluble beta blockers do not affect sleep, but fat-soluble beta blockers can interfere with sleep.
People who take fat-soluble beta blockers may wake up frequently at night, experience more nightmares, and struggle to fall back asleep. Both types of beta blockers reduce the amount of time spent in REM sleep. Independent of their effect on sleep, beta blockers may also cause daytime sleepiness.
Anti-Inflammatory Corticosteroids
Corticosteroids, particularly glucocorticoids, are often used to treat a variety of health conditions, including lung diseases, allergies, inflammatory disorders, autoimmune conditions, and some cancers. Common steroid drugs, such as prednisone and prednisolone, may be taken orally, injected, inhaled, or applied to the skin.
Sleep problems are common among people who take corticosteroids, especially those who take their medication twice a day or at night. Sleep troubles may happen because steroid drugs disrupt the body’s hormone production patterns.
Although corticosteroids are generally viewed as medications that affect sleep, not enough research has been conducted to determine how these drugs cause sleep disruptions. People who take steroids often report waking up frequently at night. Corticosteroids may also trigger mania, a mood condition that causes a person to require less sleep.
Dopamine Agonists (Parkinson's Disease Medications)
Dopamine agonists are used to treat mild or moderate Parkinson’s disease and certain mental health conditions. These medications activate dopamine receptors in the brain.
Dopamine agonists can cause daytime sleepiness and help people fall asleep faster. Some may alter sleep architecture by preventing REM sleep and lengthening the amount of time spent in stage 3 sleep.
Although dopamine agonists make many people feel more tired, these drugs are also associated with insomnia in some studies. Also, dopamine agonists can cause side effects, like nausea, vomiting, and dizziness, that may keep a person up at night.
Nicotine Replacement Treatments
Nicotine replacement therapy helps people quit smoking. Nicotine replacement aids come in the forms of gum, a patch, an inhaler, lozenges, or nasal spray. These treatments deliver nicotine into the bloodstream and prevent cravings and withdrawal symptoms.
Nicotine is known to make people more alert. Nicotine also increases blood pressure and heart rate. Those who try to quit smoking may experience trouble sleeping, nightmares, and restlessness as their bodies adjust. However, some kinds of nicotine replacement aids can also make it harder to fall asleep.
A nicotine replacement treatment’s side effects depend on how it delivers nicotine, the dosage, and the formulation. Inhalers, for example, do not usually cause sleep disturbances. Other forms, such as the patch or gum, may cause sleep problems, vivid dreams, and nightmares.
Some nicotine replacement treatments also have side effects that may keep a person awake, including nasal congestion, heartburn, and headaches.
Sleeping Pills
You might be surprised to find sleeping pills on a list of medications that cause insomnia. But, drugs that are intended to treat sleeplessness can cause unwanted side effects in some people.
Most prescription sleeping pills are categorized as benzodiazepines or nonbenzodiazepines. Both types of medication can help people fall asleep and stay asleep. They reduce time spent in stage 1 sleep, which is the lightest stage, allowing the sleeper to get better quality rest.
These sleep medications may complicate sleep for some individuals. For example, benzodiazepines can worsen symptoms of obstructive sleep apnea.
In addition, some people who take prescription sleeping pills find themselves sleepwalking or performing actions like driving, talking, and eating while they are not fully awake. Researchers estimate that up to 25% of people who use nonbenzodiazepines experience these behaviors, particularly those who take higher doses of a medication.
People who stop taking prescription sleeping pills may experience rebound insomnia. Rebound insomnia causes a person to have more difficulty falling or staying asleep after going off of a medication than they did before taking it.
Over-the-counter sleeping pills, like doxylamine and diphenhydramine, also have risks and should only be used in the short-term under the guidance of a medical professional.
Dietary Supplements
Melatonin is a supplement that may help people with insomnia fall asleep faster and maintain healthy sleep patterns. However, it does not help a sleeper stay asleep, so they may find themselves waking up in the night, even if they initially fell asleep easily. Melatonin can also disturb sleep by causing nightmares and vivid dreams.
Sometimes people opt to take a B complex vitamin to help manage sleep troubles. Research studies of B vitamins are mixed. Although one study found that B complex could successfully treat insomnia when used in combination with other treatments, like melatonin, other studies have found that it actually increases insomnia symptoms. More research is likely needed.
While there are a host of natural products and herbal supplements on the market that claim to treat insomnia, there is little evidence that these remedies are effective. A series of studies found that common herbal medicines, like valerian, did not significantly improve symptoms of insomnia, although some participants reported side effects.
Talk to a Doctor and Improve Your Sleep
Over-the-counter medications, supplements, and prescription drugs that cause insomnia are common. If you suspect your medication is affecting your sleep patterns, contact your doctor about your concerns.
Your doctor may be able to adjust your dosage, offer advice on how to cope with side effects, provide alternative treatments, or give you additional medications or supplements to help with sleep. Do not stop taking a prescribed medication without consulting your doctor first.
References
Ask the Sleep Doctor
Have questions about sleep? Submit them here! We use your questions to help us decide topics for articles, videos, and newsletters. We try to answer as many questions as possible. You can also send us an email. Please note, we cannot provide specific medical advice, and always recommend you contact your doctor for any medical matters.